Subdural Hemorrhage
- Home
- Subdural Hemorrhage
What is Subdural Hemorrhage
Subdural hemorrhage can lead to significant neurological deficits and life-threatening complications if not promptly addressed. Common causes include head trauma, coagulopathy, and rupture of an underlying vascular lesion.
Symptoms of Subdural Hemorrhage
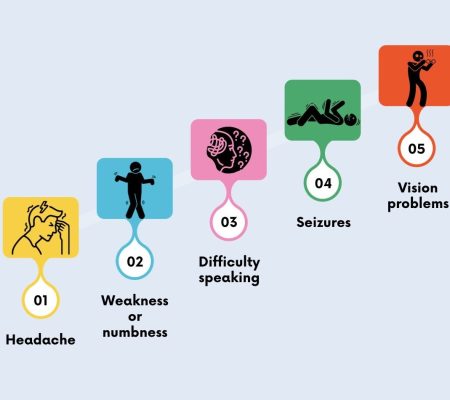
- Persistent headache that may be more severe than usual
- Confusion
- Weakness or numbness on one side of the body
- Drowsiness
- Speech and comprehension problems
- Dizziness & Seizures
- Nausea or vomiting
Embolization of the MMA enables rapid cessation of bleeding, reducing the risk of hematoma expansion
Embolization of Middle Meningeal Artery (MMA)
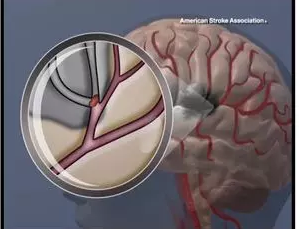
Benefits of MMA Embolization
Rapid Hemostasis
Customized Treatment
Frequently Asked Questions
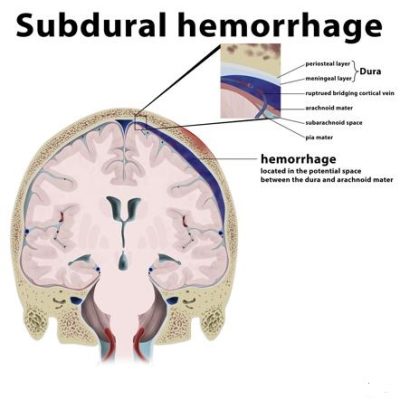
A subdural hemorrhage is a type of bleeding that occurs between the dura mater (the outermost layer covering the brain) and the arachnoid mater (the middle layer). It can result from traumatic injury or spontaneous rupture of blood vessels.
Symptoms may include headache, confusion, dizziness, nausea, vomiting, weakness, numbness, difficulty speaking, seizures, and loss of consciousness. In some cases, symptoms may develop gradually over time.
Diagnosis typically involves a combination of medical history review, physical examination, and neuroimaging studies such as CT (computed tomography) or MRI (magnetic resonance imaging) scans. These imaging studies can help identify the presence, location, and extent of the hemorrhage.
Treatment depends on various factors, including the size and severity of the hemorrhage, the patient’s overall health, and the presence of any underlying conditions. Options may include observation, medications to reduce swelling or prevent seizures, surgical drainage, or minimally invasive procedures such as embolization.
Embolization may be used as a minimally invasive treatment option for certain cases of subdural hemorrhage, particularly those caused by vascular abnormalities or bleeding from meningeal arteries. During the procedure, tiny particles or coils are injected into the blood vessels to block blood flow to the hemorrhage site, helping to control bleeding and promote resolution.
Recovery varies depending on factors such as the severity of the hemorrhage, the effectiveness of treatment, and the patient’s overall health. In some cases, patients may require rehabilitation to regain lost function or address any neurological deficits. Close follow-up with a healthcare provider is essential to monitor progress and ensure optimal recovery.

